Introduction
Langerhans cell histiocytosis (LCH) is a clonal histiocytic neoplasm, which arises when myeloid precursors expressing CD207 (Langerin) and CD1a expand and circulate as mature dendritic cells, clinically manifesting in multisystemic eosinophilic granulomas at osseous sites (notably the cranium), lungs, cutaneous tissue, and visceral structures (pituitary gland, liver, spleen). Molecular alterations in MAP kinase signaling are common, specifically in BRAFV600E, which is identified in greater than 50% of patients. Limited LCH is commonly managed with local therapies, such as surgery and radiation, while disseminated disease is managed with systemic therapies, including multi-agent chemotherapy or targeted agents, such as BRAF inhibitors. While diagnostic and management paradigms are well-established in LCH, clinical studies evaluating indicators of disease progression are lacking.
Methods
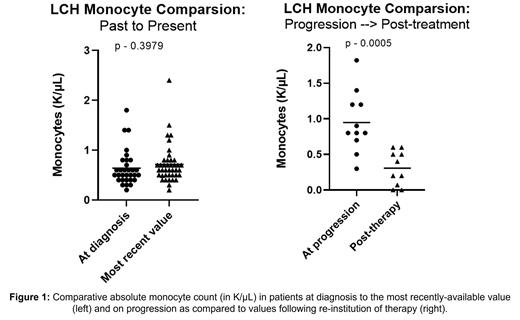
Clinical, laboratory, radiographic and treatment data for 49 patients with a histopathologic diagnosis of Langerhans Cell Histiocytosis treated at a single institution over a 20-year period was reviewed by multiple study investigators. Specific parameters reviewed included biological sex, age at and time to diagnosis, molecular diagnostic data by immunohistochemistry and/or next generation sequencing, diagnostic imaging utilized, treatment rendered, clinical and/or radiographic response. Radiography in all but 1/49 patients was used to assess treatment responses, by RECIST 1.1 where MRI, or CT was utilized and PERCIST for serial PET imaging. The peripheral blood absolute monocyte count (in K/µL) was also assessed in each patient at various timepoints, including at initial diagnosis and the most recent value. We also performed a more focused assessment of absolute monocytes at the time of disease progression (when applicable) and again following reinstitution of therapy. Statistical analyses to compare sets of data were conducted using unpaired two-sided t-tests.
Results
Of the 49 patients included in this analysis, 28 were female and 21 male, with an average age at diagnosis of approximately 38 years; time between symptom onset and diagnosis varied widely across the cohort but was generally less than 12 months. Molecular diagnostics were employed in only 8/49 patients, 3 by IHC, 4 by NGS and 1 by both; BRAFV600E was assessed in 6 patients and was positive in 2. Approach to imaging at diagnosis and throughout treatment varied but most commonly included conventional CT (25), followed by MRI (17) and PET (16). LCH was observed as a primary pulmonary disease in 18 patients (36.7%), as involvement of skull/CNS/ocular structures in 10 and as localized cutaneous involvement in 5. Complete responses were observed in 17 of 49 patients, 11/17 of whom underwent local therapy (radiation and/or surgery) at ≥1 point in his or her treatment course. On the other end of the spectrum, 5 patients never achieved any response and always had progressive/persistent disease, all of whom had been diagnosed with pulmonary LCH in the setting of chronic tobacco use. Peripheral blood absolute monocyte count between the earliest-assessed timepoint and latest value, lastly, did not differ. The mean value on progression (0.94 K/µL), however, was significantly higher than that following re-institution of therapy (0.31, p=0.0005) as depicted in Figure 1.
Discussion
The identification of relative monocytosis at the time of LCH progression was an unexpected finding in this study. LCH pathogenesis has been felt to berelated to dysregulated hematopoiesis and acquisition of somatic mutations during monocyte differentiation, ultimately driving clonal expansion of CD1a+/CD207+ histiocytes. Within this working model of disruption to monocyte differentiation, one explanation of our observed findings is a simple expansion in circulating monocytes as a manifestation of disease progressing throughout various tissues. Another possibility is that circulating monocytes are upregulated and later differentiate into mature dendritic cells for MHC Class I presentation. Similar observations have been made at our institution in cohorts of non-LCH histiocytosis, specifically Rosai Dorfman and Erdheim Chester Disease. Expanded integrated genomic-transcriptomic sequencing analyses to evaluate the molecular character of LCH and ultimately clarify the origin of this monocyte trend are currently underway.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal